- Research
- Open access
- Published:
Research landscape analysis on dual diagnosis of substance use and mental health disorders: key contributors, research hotspots, and emerging research topics
Annals of General Psychiatry volume 23, Article number: 32 (2024)
Abstract
Background
Substance use disorders (SUDs) and mental health disorders (MHDs) are significant public health challenges with far-reaching consequences on individuals and society. Dual diagnosis, the coexistence of SUDs and MHDs, poses unique complexities and impacts treatment outcomes. A research landscape analysis was conducted to explore the growth, active countries, and active journals in this field, identify research hotspots, and emerging research topics.
Method
A systematic research landscape analysis was conducted using Scopus to retrieve articles on dual diagnosis of SUDs and MHDs. Inclusion and exclusion criteria were applied to focus on research articles published in English up to December 2022. Data were processed and mapped using VOSviewer to visualize research trends.
Results
A total of 935 research articles were found. The number of research articles on has been increasing steadily since the mid-1990s, with a peak of publications between 2003 and 2012, followed by a fluctuating steady state from 2013 to 2022. The United States contributed the most articles (62.5%), followed by Canada (9.4%). The Journal of Dual Diagnosis, Journal of Substance Abuse Treatment, and Mental Health and Substance Use Dual Diagnosis were the top active journals in the field. Key research hotspots include the comorbidity of SUDs and MHDs, treatment interventions, quality of life and functioning, epidemiology, and the implications of comorbidity. Emerging research topics include neurobiological and psychosocial aspects, environmental and sociocultural factors, innovative interventions, special populations, and public health implications.
Conclusions
The research landscape analysis provides valuable insights into dual diagnosis research trends, active countries, journals, and emerging topics. Integrated approaches, evidence-based interventions, and targeted policies are crucial for addressing the complex interplay between substance use and mental health disorders and improving patient outcomes.
Introduction
Substance use disorders (SUDs) refer to a range of conditions characterized by problematic use of psychoactive substances, leading to significant impairment in physical, psychological, and social functioning [1]. These substances may include alcohol, tobacco, illicit drugs (e.g., cocaine, opioids, cannabis), and prescription medications. The global burden of SUDs is substantial, with far-reaching consequences on public health, socio-economic development, and overall well-being. For instance, alcohol abuse accounts for 3 million deaths worldwide annually, while the opioid crisis has escalated to unprecedented levels in certain regions, such as North America, resulting in tens of thousands of overdose deaths per year [2,3,4]. Mental health disorders (MHDs) encompass a wide range of conditions that affect mood, thinking, behavior, and emotional well-being [5]. Examples of MHDs include depression, anxiety disorders, post-traumatic stress disorder (PTSD), bipolar disorder, schizophrenia, and eating disorders. These conditions can significantly impair an individual's ability to function, negatively impacting their quality of life, relationships, and overall productivity [6,7,8]. Furthermore, certain MHD such as major depressive disorder and anxiety are often associated with specific affective temperaments, hopelessness, and suicidal behavior and grasping such connections can help in crafting customized interventions to reduce suicide risk [9]. In addition, a systematic review of 18 studies found that demoralization with somatic or psychiatric disorders is a significant independent risk factor for suicide and negative clinical outcomes across various populations [10]. The coexistence of SUDs and MHDs, often referred to as dual diagnosis or comorbidity, represents a complex and prevalent phenomenon that significantly impacts affected individuals and healthcare systems [11,12,13,14,15]. For instance, individuals with depression may be more likely to self-medicate with alcohol or drugs to cope with emotional distress [16]. Similarly, PTSD has been linked to increased rates of substance abuse, as individuals attempt to alleviate the symptoms of trauma [17, 18]. Moreover, chronic substance use can lead to changes in brain chemistry, increasing the risk of developing MHDs or exacerbating existing conditions [17, 19,20,21]. The coexistence of SUDs and MHDs presents unique challenges from a medical and clinical standpoint. Dual diagnosis often leads to more severe symptoms, poorer treatment outcomes, increased risk of relapse, and higher rates of hospitalization compared to either disorder alone [22]. Additionally, diagnosing and treating dual diagnosis cases can be complex due to overlapping symptoms and interactions between substances and psychiatric medications. Integrated treatment approaches that address both conditions simultaneously are essential for successful recovery and improved patient outcomes [20]. Patients grappling with dual diagnosis encounter a multifaceted web of barriers when attempting to access essential mental health services. These barriers significantly compound the complexity of their clinical presentation. The first barrier pertains to stigma, where societal prejudices surrounding mental health and substance use disorders deter individuals from seeking help, fearing discrimination or social repercussions [23]. A lack of integrated care, stemming from fragmented healthcare systems, poses another significant hurdle as patients often struggle to navigate separate mental health and addiction treatment systems [24]. Insurance disparities contribute by limiting coverage for mental health services and imposing strict criteria for reimbursement [25]. Moreover, there is a shortage of adequately trained professionals equipped to address both substance use and mental health issues, creating a workforce barrier [26]. Geographical disparities in access further hinder care, particularly in rural areas with limited resources [27]. These barriers collectively serve to exacerbate the clinical complexity of patients with dual diagnosis, and ultimately contributing to poorer outcomes.
A research landscape analysis involves a systematic review and synthesis of existing literature on a specific topic to identify key trends, knowledge gaps, and research priorities [28, 29]. Scientific research landscape analysis, is motivated by various factors. First, the rapid growth of scientific literature poses a challenge for researchers to stay up-to-date with the latest developments in their respective fields. Research landscape analysis provides a structured approach to comprehend the vast body of literature, identifying crucial insights and emerging trends. Additionally, it plays a vital role in identifying knowledge gaps, areas with limited research, or inadequate understanding. This pinpointing allows researchers to focus on critical areas that demand further investigation, fostering more targeted and impactful research efforts [30]. Furthermore, in the realm of policymaking and resource allocation, evidence-based decision-making is crucial. Policymakers and funding agencies seek reliable information to make informed decisions about research priorities. Research landscape analysis offers a comprehensive view of existing evidence, facilitating evidence-based decision-making processes [28]. When it comes to the research landscape analysis of dual diagnosis of SUDs and MHDs, there are several compelling justifications to explore this complex comorbidity and gain a comprehensive understanding of its interplay and impact on patient outcomes. Firstly, the complexity of the interplay between SUDs and MHDs demands a comprehensive examination of current research to unravel the intricacies of this comorbidity [31]. Secondly, dual diagnosis presents unique challenges for treatment and intervention strategies due to the overlapping symptoms and interactions between substances and psychiatric medications. A research landscape analysis can shed light on effective integrated treatment approaches and identify areas for improvement [18]. Moreover, the public health impact of co-occurring SUDs and MHDs is substantial, resulting in more severe symptoms, poorer treatment outcomes, increased risk of relapse, and higher rates of hospitalization. Understanding the research landscape can inform public health policies and interventions to address this issue more effectively [32]. Lastly, the holistic approach of research landscape analysis enables a comprehensive understanding of current knowledge, encompassing epidemiological data, risk factors, treatment modalities, and emerging interventions. This integrative approach can lead to more coordinated and effective care for individuals with dual diagnosis [22]. Based on the above argument, the current study aims to conduct a research landscape analysis of dual diagnosis of SUDs and MHDs. The research landscape analysis bears a lot of significance for individuals and society. First and foremost, it’s a beacon of hope for individuals seeking help. Research isn’t just about dry statistics; it's about finding better ways to treat and support those facing dual diagnosis. By being informed about the latest breakthroughs, healthcare professionals can offer more effective, evidence-backed care, opening the door to improved treatment outcomes and a brighter future for those they serve. Beyond the individual level, this understanding has profound societal implications. It has the power to chip away at the walls of stigma that often surround mental health and substance use issues. Greater awareness and knowledge about the complexities of dual diagnosis can challenge stereotypes and biases, fostering a more compassionate and inclusive society. Additionally, society allocates resources based on research findings. When we understand the prevalence and evolving nature of dual diagnosis, policymakers and healthcare leaders can make informed decisions about where to channel resources most effectively. This ensures that the needs of individuals struggling with co-occurring disorders are not overlooked or under-prioritized. Moreover, research helps identify risk factors and early warning signs related to dual diagnosis. Armed with this information, we can develop prevention strategies and early intervention programs, potentially reducing the incidence of co-occurring disorders and mitigating their impact. Legal and criminal justice systems also stand to benefit. Understanding dual diagnosis trends can inform policies related to diversion programs, treatment alternatives to incarceration, and the rehabilitation of individuals with co-occurring disorders, potentially reducing rates of reoffending. Moreover, dual diagnosis research contributes to public health planning by highlighting the need for integrated mental health and addiction services. This knowledge can guide the development of comprehensive healthcare systems that offer holistic care to individuals with co-occurring disorders. Families and communities, too, are vital players in this narrative. With a grasp of research findings, they can provide informed, empathetic, and effective support to their loved ones, contributing to better outcomes.
Methods
The present research landscape analysis of dual diagnosis of SUDs and MHDs was conducted using a systematic approach to retrieve, process, and analyze relevant articles. The following methodology outlines the key steps taken to address the research questions:
Research Design The present study constitutes a thorough and robust analysis of the research landscape concerning the dual diagnosis of SUD and MHD. It's important to note that the research landscape analysis differs from traditional systematic or scoping reviews. In conducting research landscape analysis, we made deliberate methodological choices aimed at achieving both timely completion and unwavering research quality. These choices included a strategic decision to focus our search exclusively on a single comprehensive database, a departure from the customary practice of utilizing multiple databases. Furthermore, we streamlined the quality control process by assigning specific quality checks to a single author, rather than following the conventional dual-reviewer approach. This approach prioritized efficiency and expediency without compromising the rigor of our analysis. To expedite the research process further, we opted for a narrative synthesis instead of a quantitative one, ensuring that we provide a succinct yet highly informative summary of the available evidence. We place a premium on research transparency and, as such, are committed to sharing the detailed search string employed for data retrieval. This commitment underscores our dedication to fostering reproducibility and transparency in research practices.
Ethical considerations Since the research landscape analysis involved the use of existing and publicly available literature, and no human subjects were directly involved, no formal ethical approval was required.
Article retrieval Scopus, a comprehensive bibliographic database, was utilized to retrieve articles related to the dual diagnosis of SUDs and MHDs. Scopus is a multidisciplinary abstract and citation database that covers a wide range of scientific disciplines, including life sciences, physical sciences, social sciences, and health sciences. It includes content from thousands of scholarly journals.
Keywords used To optimize the search process and ensure the inclusion of pertinent articles, a set of relevant keywords and equivalent terms were employed. Keywords for “dual diagnosis” included dual diagnosis, co-occurring disorders, comorbid substance use, comorbid addiction, coexisting substance use, combined substance use, simultaneous substance use, substance use and psychiatric, co-occurring substance use and psychiatric, concurrent substance use and mental, coexisting addiction and mental, combined addiction and mental, simultaneous addiction and mental, substance-related and psychiatric, comorbid mental health and substance use, co-occurring substance use and psychiatric, concurrent mental health and substance use, coexisting mental health and substance use, combined mental health and substance use, simultaneous mental health and substance use, substance-related and coexisting psychiatric, comorbid psychiatric and substance abuse, co-occurring mental health and substance-related, concurrent psychiatric and substance use, coexisting psychiatric and substance abuse, combined psychiatric and substance use, simultaneous psychiatric and substance use, substance-related and concurrent mental, substance abuse comorbidity. Keywords for “Substance use disorders” included substance abuse, substance dependence, drug use disorders, addiction, substance-related disorders, drug abuse, opioid use disorder, cocaine use disorder, alcohol use disorder, substance misuse, substance use disorder, substance-related, substance addiction. Keywords for “Mental health disorders” included psychiatric disorders, mental illnesses, mental disorders, emotional disorders, psychological disorders, schizophrenia, depression, PTSD, ADHD, anxiety, bipolar disorder, eating disorders, personality disorders, mood disorders, psychotic disorders, mood and anxiety disorders, mental health conditions. To narrow down the search to focus specifically on dual diagnosis, we adopted a strategy that involved the simultaneous presence of SUDs and MHDs in the presence of specific keywords in the titles and abstracts such as “dual,” “co-occurring,” “concurrent,” “co-occurring disorders,” “dual disorders,” “dual diagnosis,” “comorbid psychiatric,” “cooccurring psychiatric,” “comorbid*,” and “coexisting”.
Inclusion and exclusion criteria To maintain the study’s focus and relevance, specific inclusion and exclusion criteria were applied. Included articles were required to be research article, written in English, and published in peer-reviewed journals up to December 31, 2022, Articles focusing on animal studies, internet addiction, obesity, pain, and validity of instruments and tools were excluded.
Flow chart of the search strategy Supplement 1 shows the overall search strategy and the number of articles retrieved in each step. The total number of research articles that met the inclusion and exclusion criteria were 935.
Validation of search strategy The effectiveness of our search strategy was rigorously assessed through three distinct methods, collectively demonstrating its ability to retrieve pertinent articles while minimizing false positives. First, to gauge precision, we meticulously examined a sample of 30 retrieved articles, scrutinizing their alignment with our research question and their contributions to the topic of dual diagnosis. This manual review revealed that the majority of the assessed articles were highly relevant to our research focus. Second, for a comprehensive evaluation, we compared the articles obtained through our search strategy with a set of randomly selected articles from another source. This set comprised 10 references sourced from Google Scholar [33,34,35,36,37,38,39,40,41,42], and the aim was to determine if our strategy successfully identified articles selected at random from an alternative database. Impressively, our analysis showed that the search strategy had a notably high success rate in capturing these randomly selected articles. Lastly, to further corroborate the relevance of our retrieved articles, we investigated the research interests of the top 10 active authors and the subject scope of the top 10 active journals. This exploration confirmed that their areas of expertise and the journal scopes were in alignment with the field of mental health and/or substance use disorders. These three validation methods collectively reinforce the reliability of our search strategy, affirming that the vast majority of the retrieved articles are indeed pertinent to our research inquiry.
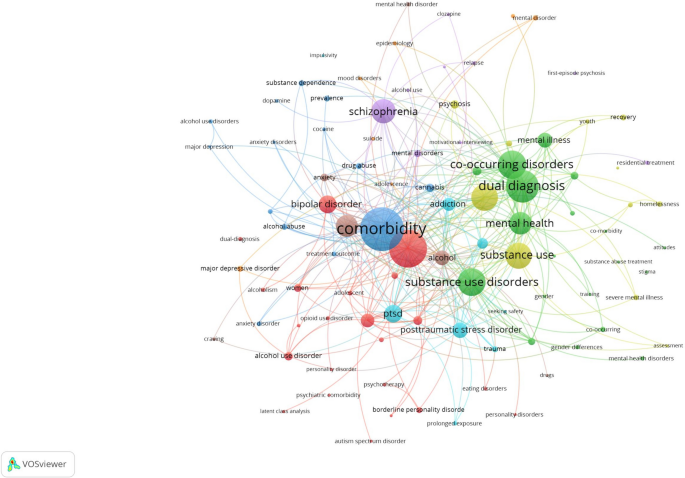
Data processing and mapping Data extracted from the selected articles were processed and organized using Microsoft Excel. Information on the titles/abstracts/author keywords, year of publication, journal name, authors, institution and country affiliation, and number of citations received by the article were extracted. To visualize and analyze the research landscape, VOSviewer, a bibliometric analysis tool, was employed [43]. This software enables mapping and clustering of co-occurring terms, authors, and countries, providing a comprehensive overview of the dual diagnosis research domain.
Interpreting VOSviewer maps and generating research topics
We conducted a rigorous analysis and generated a comprehensive research landscape using VOSviewer, a widely acclaimed software tool renowned for its expertise in mapping research domains. We seamlessly integrated pertinent data extracted from the Scopus database, including publication metadata, into VOSviewer to delve into the frequency of author keywords and terminologies. The resulting visualizations provided us with profound insights into the intricate web of interconnected research topics and their relationships within the field. Interpreting VOSviewer maps is akin to navigating a vibrant and interconnected tapestry of knowledge. Each term or keyword in the dataset is depicted as a point on the map, represented by a circle or node. These nodes come in varying sizes and colors and are interconnected by lines of differing thicknesses. The size of a node serves as an indicator of the term’s significance or prevalence within the dataset. Larger nodes denote that a specific term is frequently discussed or plays a pivotal role in the body of research, while smaller nodes signify less commonly mentioned concepts. The colors assigned to these nodes serve a dual purpose. Firstly, they facilitate the categorization of terms into thematic groups, with terms of the same color typically belonging to the same cluster or sharing a common thematic thread. Secondly, they aid in the identification of distinct research clusters or thematic groups within the dataset. For instance, a cluster of blue nodes might indicate that these terms are all associated with a particular area of research. The spatial proximity of nodes on the map reflects their closeness in meaning or concept. Nodes positioned closely together share a robust semantic or contextual connection and are likely to be co-mentioned in research articles or share a similar thematic focus. Conversely, nodes situated farther apart indicate less commonality in terms of their usage in the literature. The lines that link these nodes represent the relationships between terms. The thickness of these lines provides insights into the strength and frequency of these connections. Thick lines indicate that the linked terms are frequently discussed together or exhibit a robust thematic association, while thinner lines imply weaker or less frequent connections. In essence, VOSviewer maps offer a visual narrative of the underlying structure and relationships within your dataset. By examining node size and color, you can pinpoint pivotal terms and thematic clusters. Simultaneously, analyzing the distance between nodes and line thickness unveils the semantic closeness and strength of associations between terms. These visual insights are invaluable for researchers seeking to unearth key concepts, identify research clusters, and track emerging trends within their field of study.
Results
Growth pattern, active countries, and active journals
The growth pattern of the 935 research articles on dual diagnosis of substance use disorders and mental health disorders shows an increasing trend in the number of published articles over the years. Starting from the late 1980s and early 1990s with only a few publications, the research interest gradually picked up momentum, and the number of articles has been consistently rising since the mid-1990s. Table 1 shows the number of articles published in three different periods. The majority of publications (52.2%) were produced between 2003 and 2012, indicating a significant surge in research during that decade. The subsequent period from 2013 to 2022 saw a continued interest in the subject, accounting for 35.5% of the total publications. The number of articles published per year during the period from 2013 to 2022 showed a fluctuating steady state with an average of approximately 33 articles per year. The earliest period from 1983 to 2002 comprised 12.3% of the total publications, reflecting the initial stages of research and the gradual development of interest in the field.
Out of the total 935 publications, the United States contributed the most with 585 publications, accounting for approximately 62.5% of the total research output. Canada follows with 88 publications, making up around 9.4% of the total. The United Kingdom and Australia also made substantial contributions with 70 and 53 publications, accounting for 7.5 and 5.7%, respectively. Table 2 shows the top 10 active countries.
Based on the list of top active journals in the field of dual diagnosis of substance use and mental health disorders, it is evident that there are several reputable and specialized journals that focus on this important area of research (Table 3). These journals cover a wide range of topics related to dual diagnosis, including comorbidity, treatment approaches, intervention strategies, and epidemiological studies. The Journal of Dual Diagnosis appears to be a leading and comprehensive platform for research on dual diagnosis. It covers a broad spectrum of studies related to substance use disorders and mental health conditions. The Journal of Substance Abuse Treatment ranked second while the Mental Health and Substance Use Dual Diagnosis journal ranked third and seems to be dedicated specifically to the intersection of substance use disorder and mental health disorders, providing valuable insights and research findings related to comorbidities and integrated treatment approaches.
Most frequent author keywords
Mapping author keywords with a minimum occurrence of five (n = 96) provides insights in research related to dual diagnosis. Figure 1 shows the 96 author keywords and their links with other keywords. The number of occurrences represent the number of times each author keyword appears in the dataset, while the total link strength (TLS) indicates the combined strength of connections between keywords based on their co-occurrence patterns. The most frequent author keywords with high occurrences and TLS represent the key areas of focus in research on the dual diagnosis of substance use and mental health disorders.
-
1.
“Comorbidity” is the most frequent keyword, with 144 occurrences and a high TLS of 356. This reflects the central theme of exploring the co-occurrence of substance use disorders and mental health conditions and their complex relationship. “Substance use disorder” and “dual diagnosis” are also highly prevalent keywords with 122 and 101 occurrences, respectively. These terms highlight the primary focus on studying individuals with both substance use disorders and mental health disorders, underscoring the significance of dual diagnosis in research. “Co-occurring disorders” and “substance use disorders” are frequently used, indicating a focus on understanding the relationship between different types of disorders and the impact of substance use on mental health. Several specific mental health disorders such as “schizophrenia,” “depression,” “bipolar disorder,” and “PTSD” are prominent keywords, indicating a strong emphasis on exploring the comorbidity of these disorders with substance use. “Mental health” and “mental illness” are relevant keywords, reflecting the broader context of research on mental health conditions and their interaction with substance use. “Treatment” is a significant keyword with 34 occurrences, indicating a focus on investigating effective interventions and treatment approaches for individuals with dual diagnosis. “Addiction” and “recovery” are important keywords, highlighting the interest in understanding the addictive nature of substance use and the potential for recovery in this population. The mention of “veterans” as a keyword suggests a specific focus on the dual diagnosis of substance use and mental health disorders in the veteran population. “Integrated treatment” is an important keyword, indicating an interest in studying treatment approaches that address both substance use and mental health disorders together in an integrated manner.
Most impactful research topics
To have an insight into the most impactful research topics on dual diagnosis, the top 100 research articles were visualized and the terms with the largest node size and TLS were used to. To come up with the five most common investigated research topics:
-
1.
Dual diagnosis and comorbidity of SUDs and MHDs: This topic focuses on the co-occurrence of substance use disorders and various mental health conditions, such as schizophrenia, bipolar disorder, PTSD, anxiety disorders, and major depressive disorder. This research topic explored the prevalence, characteristics, and consequences of comorbidity in different populations, including veterans, adolescents, and individuals experiencing homelessness [13, 19, 44,45,46,47,48,49,50,51,52].
-
2.
Treatment and interventions for co-occurring disorders: This topic involves studies on different treatment approaches and interventions for individuals with dual diagnosis. These interventions may include motivational interviewing, cognitive-behavioral therapy, family intervention, integrated treatment models, assertive community treatment, and prolonged exposure therapy. The goal is to improve treatment outcomes and recovery for individuals with co-occurring substance use and mental health disorders [48, 53,54,55,56,57,58,59].
-
3.
Quality of life and functioning in individuals with dual diagnosis: This research topic explores the impact of dual diagnosis on the quality of life and functioning of affected individuals. It assesses the relationship between dual diagnosis and various aspects of well-being, including social functioning, physical health, and overall quality of life [60,61,62,63,64].
-
4.
Epidemiology and prevalence of co-occurring disorders: This topic involves population-based studies that investigate the prevalence of comorbid substance use and mental health disorders. It examines the demographic and clinical correlates of dual diagnosis, as well as risk factors associated with the development of co-occurring conditions [50, 52, 60, 65,66,67].
-
5.
Implications and consequences of comorbidity: This research topic explores the consequences of comorbidity between substance use and mental health disorders, such as treatment utilization, service access barriers, criminal recidivism, and the impact on suicidality. It also investigates the implications of comorbidity for treatment outcomes and the potential risks associated with specific comorbidities [68,69,70,71,72,73,74,75].
Emerging research topics
Upon scrutinizing the titles, abstracts, author keywords, and a visualization map of the 100 recently published articles, the research themes listed below came to the forefront. It’s worth noting that some of the research themes in the 100 recently published articles were not groundbreaking; rather, they represented a natural progression of ongoing research endeavors, and that is why they were not listed as emerging research themes. For instance, there was a continuation of research into the prevalence and epidemiology of co-occurring mental illnesses and substance use disorders and characteristics of various cases of co-morbid cases of SUDs and MHDs. The list below included such emergent themes. It might seem that certain aspects within these research themes duplicate the initial research topics, but it’s crucial to emphasize that this is not the case. For example, both themes delve into investigations concerning treatment, yet the differentiation lies in the treatment approach adopted.
-
1.
Neurobiological and psychosocial aspects of dual diagnosis: This research topic focuses on exploring the neurobiological etiology and underlying mechanisms of comorbid substance use and mental health disorders. It investigates brain regions, neurotransmitter systems, hormonal pathways, and other neurobiological factors contributing to the development and maintenance of dual diagnosis. Additionally, this topic may examine psychosocial aspects, such as trauma exposure, adverse childhood experiences, and social support, that interact with neurobiological factors in the context of comorbidity [76].
-
2.
Impact of environmental and sociocultural factors on dual diagnosis: This research topic delves into the influence of environmental and sociocultural factors on the occurrence and course of comorbid substance use and mental health disorders. It may explore how cultural norms, socioeconomic status, access to healthcare, and societal attitudes toward mental health and substance use affect the prevalence, treatment outcomes, and quality of life of individuals with dual diagnosis [77, 78].
-
3.
New interventions and treatment approaches for dual diagnosis: This topic involves studies that propose and evaluate innovative interventions and treatment approaches for individuals with dual diagnosis. These interventions may include novel psychotherapeutic techniques, pharmacological treatments, digital health interventions, and integrated care models. The research aims to improve treatment effectiveness, adherence, and long-term recovery outcomes in individuals with comorbid substance use and mental health disorders [79,80,81,82,83,84].
-
4.
Mental health and substance use in special populations with dual diagnosis: This research topic focuses on exploring the prevalence and unique characteristics of comorbid substance use and mental health disorders in specific populations, such as individuals with eating disorders, incarcerated individuals, and people with autism spectrum disorder. It aims to identify the specific needs and challenges faced by these populations and develop tailored interventions to address their dual diagnosis [85,86,87,88,89,90,91,92,93,94,95].
-
5.
Public health implications and policy interventions for dual diagnosis: This topic involves research that addresses the public health implications of dual diagnosis and the need for policy interventions to address this complex issue. It may include studies on the economic burden of comorbidity, the impact on healthcare systems, and the evaluation of policy initiatives aimed at improving prevention, early intervention, and access to integrated care for individuals with dual diagnosis [81, 96,97,98,99,100,101].
Comparison in research topics
The comparison between the most impactful research topics and emerging research topics in the field of dual diagnosis reveals intriguing insights into the evolving landscape of this critical area of study (Table 4). In the most impactful research topics, there is a strong emphasis on the epidemiology of dual diagnosis, indicating a well-established foundation in understanding the prevalence, characteristics, and consequences of comorbid SUDs and MHDs. Treatment and interventions also receive considerable attention, highlighting the ongoing efforts to improve outcomes and recovery for individuals with dual diagnosis. Quality of life and medical consequences are additional focal points, reflecting the concern for the holistic well-being of affected individuals and the health-related implications of comorbidity.
On the other hand, emerging research topics signify a shift towards newer methods and interventions. The exploration of neurobiology in the context of dual diagnosis reflects a growing interest in unraveling the underlying neurobiological mechanisms contributing to comorbidity. This shift suggests a deeper understanding of the neural pathways and potential targets for intervention. The consideration of dual diagnosis in special groups underscores a recognition of the unique needs and challenges faced by specific populations, such as individuals with autism spectrum disorder. This tailored approach acknowledges that one size does not fit all in addressing dual diagnosis. Finally, the exploration of environmental and psychosocial contexts highlights the importance of socio-cultural factors, policy interventions, and societal attitudes in shaping the experience of individuals with dual diagnosis, signaling a broader perspective that extends beyond clinical interventions. In summary, while the most impactful research topics have laid a strong foundation in epidemiology, treatment, quality of life, and medical consequences, the emerging research topics point to a promising future with a deeper dive into the neurobiology of dual diagnosis, a focus on special populations, and a broader consideration of the environmental and psychosocial context. This evolution reflects the dynamic nature of dual diagnosis research as it strives to advance our understanding and improve the lives of those affected by comorbid substance use and mental health disorders.
Discussion
The main hypothesis underlying the study was that dual diagnosis, or the comorbidity of SUDs and MHDs, was historically underrecognized and under-researched. Over time, however, there has been a significant increase in understanding, appreciation, and research into this complex interplay in clinical settings. This was expected to manifest through a growing number of publications, increased attention to integrated treatment approaches, and a heightened recognition of the complexities and public health implications associated with dual diagnosis. The study aims to analyze this progression and its implications through a research landscape analysis, identifying key trends, knowledge gaps, and research priorities. The research landscape analysis of the dual diagnosis of SUDs and MHDs has unveiled a substantial and evolving body of knowledge, with a notable rise in publications since the mid-1990s and a significant surge between 2003 and 2012. This growing research interest underscores the increasing recognition of the importance and complexity of dual diagnosis in clinical and public health contexts. The United States has emerged as the most active contributor, followed by Canada, the United Kingdom, and Australia, with specialized journals such as the Journal of Dual Diagnosis playing a pivotal role in disseminating research findings. Common keywords such as “comorbidity,” “substance use disorder,” “dual diagnosis,” and specific mental health disorders highlight the primary focus areas, with impactful research topics identified as the comorbidity of SUDs and MHDs, treatment and interventions, quality of life, epidemiology, and the implications of comorbidity. Emerging research themes emphasize neurobiological and psychosocial aspects, the impact of environmental and sociocultural factors, innovative treatment approaches, and the needs of special populations with dual diagnosis, reflecting a shift towards a more holistic and nuanced understanding. The study highlights a shift from traditional epidemiological studies towards understanding the underlying mechanisms and broader social determinants of dual diagnosis, with a need for continued research into integrated treatment models, specific needs of diverse populations, and the development of tailored interventions.
The findings of this research landscape analysis have significant implications for clinical practice, public health initiatives, policy development, and future research endeavors. Clinicians and healthcare providers working with individuals with dual diagnosis can benefit from the identified research hotspots, as they highlight crucial aspects that require attention in diagnosis, treatment, and support. The prominence of treatment and intervention topics indicates the need for evidence-based integrated approaches that address both substance use and mental health disorders concurrently [102,103,104]. The research on the impact of dual diagnosis on quality of life and functioning underscores the importance of holistic care that addresses psychosocial and functional well-being [63]. For public health initiatives, understanding the prevalence and epidemiological aspects of dual diagnosis is vital for resource allocation and the development of effective prevention and early intervention programs. Policymakers can use the research landscape analysis to inform policies that promote integrated care, reduce barriers to treatment, and improve access to mental health and substance abuse services [15, 105]. Furthermore, the identification of emerging topics offers opportunities for investment in research areas that are gaining momentum and importance.
The present study lays a robust groundwork, serving as a catalyst for the advancement of research initiatives and the formulation of comprehensive policies and programs aimed at elevating the quality of life for individuals grappling with the intricate confluence of SUDs and MHDs. Within the realm of significance, it underscores a critical imperative—the urgent necessity to revolutionize the landscape of tailored mental health services offered to patients harboring this challenging comorbidity. The paper distinctly illuminates the exigency for a heightened quantity of research endeavors that delve deeper into unraveling the temporal intricacies underpinning the relationship between SUDs and MHDs. In so doing, it not only unveils potential risk factors but also delves into the far-reaching consequences of treatment modalities over the extended course of time. This illumination, therefore, not only beckons but virtually ushers in a promising trajectory for prospective research endeavors, a path designed to uncover the intricate and evolving journey of dual diagnosis. A profound implication of this study is the direct applicability of its findings in the corridors of policymaking. By leveraging the insights encapsulated within the paper, policymakers stand uniquely equipped to sculpt policies that unequivocally champion the cause of integrated care. The remarkable emphasis on themes of treatment and intervention, permeating the research's core, emphatically underscores the urgent demand for dismantling barriers obstructing access to mental health and substance abuse services. It is incumbent upon policymakers to heed this call, for policies fostering the integration of care can inexorably elevate the outcomes experienced by patients grappling with dual diagnosis. Furthermore, this study artfully directs policymakers to allocate their resources judiciously by identifying burgeoning areas of research that are surging in prominence and pertinence. These emergent topics, discerned within the study, are not just topics; they are emblematic of windows of opportunity. By investing in these areas, policymakers can tangibly bolster research initiatives that are primed to tackle the multifaceted challenges inherent in the realm of dual diagnosis, addressing both current exigencies and future prospects. Additionally, the paper furnishes the foundational blueprint essential for the development of screening guidelines and clinical practice protocols that truly grasp the complexity of dual diagnosis. Clinical practitioners and healthcare establishments would be remiss not to harness this invaluable information to augment their own practices, thereby delivering more effective and empathetic care to individuals contending with dual diagnosis. In essence, this study serves as the compass guiding the way toward a more compassionate, comprehensive, and efficacious approach to mental health and substance abuse care for those in need.
The current landscape analysis of reveals significant implications and highlights the growing research interest in this field since the late 1980s. This increasing trend underscores the complexities and prevalence of comorbid conditions, which necessitate focused research and intervention strategies. The results can be generalized to guide future research priorities, inform clinical guidelines, shape healthcare policies, and provide a framework for other countries to adapt and build upon in their context.
The key take-home message emphasizes the importance of recognizing the high prevalence and intricate relationship between SUDs and MHDs, necessitating integrated and tailored treatment approaches. Additionally, the study advocates for employing efficient research methodologies to synthesize vast amounts of literature and identify emerging trends, focusing on quality of life, treatment outcomes, and the broader socio-cultural and policy contexts to improve care and support for individuals with dual diagnosis. Finally, the research underscores the critical need for continued focus on dual diagnosis, advocating for comprehensive, integrated, and innovative approaches to research, clinical practice, and policymaking to improve outcomes for affected individuals.
Despite the comprehensive approach adopted in this research landscape analysis, several limitations must be acknowledged. The exclusive reliance on Scopus, while extensive, inherently limits the scope of the analysis, potentially omitting relevant articles indexed in other databases such as the Chinese scientific database, thus not fully representing the entire research landscape on dual diagnosis of SUDs and MHDs. Assigning quality control responsibilities to a single author, rather than employing a dual-reviewer system, may introduce bias and affect the reliability of the quality assessment. Although this approach was chosen to expedite the process, it might have compromised the thoroughness of quality checks. The use of narrative synthesis instead of a quantitative synthesis limits the ability to perform meta-analytical calculations that could provide more robust statistical insights. This choice was made for efficiency, but it may affect the depth of the analysis and the generalizability of the conclusions. The reliance on specific keywords to retrieve articles means that any relevant studies not containing these exact terms in their titles or abstracts may have been overlooked, potentially leading to an incomplete representation of the research domain. The restriction to English-language articles and peer-reviewed journals may exclude significant research published in other languages or in non-peer-reviewed formats, introducing linguistic and publication type bias that could skew the results towards predominantly English-speaking regions and established academic journals. The inclusion of articles up to December 31, 2022, means that any significant research published after this date is not considered, potentially missing the latest developments in the field. The validation of the search strategy using a small sample of 30 articles and a comparison with 10 randomly selected articles from Google Scholar may not be sufficient to comprehensively assess the effectiveness of the search strategy; a larger sample size might provide a more accurate validation. Some of the research topics and findings may be specific to particular populations (e.g., veterans) and might not be generalizable to other groups, highlighting the need for caution when extrapolating the results to broader contexts. Although no formal ethical approval was required due to the use of existing literature, ethical considerations related to the interpretation and application of findings must still be acknowledged, particularly in terms of representing vulnerable populations accurately and sensitively. Acknowledging these limitations is crucial for interpreting the findings of this research landscape analysis and for guiding future research efforts to address these gaps and enhance the robustness and comprehensiveness of studies on the dual diagnosis of SUDs and MHDs.
Conclusions
In conclusion, the research landscape analysis of dual diagnosis of substance abuse and mental health disorders provides valuable insights into the growth, active countries, and active journals in this field. The identification of research hotspots and emerging topics informs the scientific community about prevailing interests and potential areas for future investigation. Addressing research gaps can lead to a more comprehensive understanding of dual diagnosis, while the implications of the findings extend to clinical practice, public health initiatives, policy development, and future research priorities. This comprehensive understanding is crucial in advancing knowledge, improving care, and addressing the multifaceted challenges posed by dual diagnosis to individuals and society.
Availability of data and materials
All data presented in this manuscript are available on the Scopus database using the search query listed in the methodology section.
References
Hasin DS, O’Brien CP, Auriacombe M, Borges G, Bucholz K, Budney A, et al. DSM-5 criteria for substance use disorders: recommendations and rationale. Am J Psychiatry. 2013;170(8):834–51. https://doi.org/10.1176/appi.ajp.2013.12060782.
Collaborators GA. Alcohol use and burden for 195 countries and territories, 1990–2016: a systematic analysis for the global burden of disease study 2016. Lancet. 2018;392(10152):1015–35. https://doi.org/10.1016/s0140-6736(18)31310-2.
Ayalew M, Tafere M, Asmare Y. Prevalence, trends, and consequences of substance use among university students: implication for intervention. Int Q Community Health Educ. 2018;38(3):169–73. https://doi.org/10.1177/0272684x17749570.
Raftery D, Kelly PJ, Deane FP, Baker AL, Ingram I, Goh MCW, et al. Insight in substance use disorder: a systematic review of the literature. Addict Behav. 2020;111:106549. https://doi.org/10.1016/j.addbeh.2020.106549.
Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry. 2005;62(6):593–602. https://doi.org/10.1001/archpsyc.62.6.593.
Hossain MM, Nesa F, Das J, Aggad R, Tasnim S, Bairwa M, et al. Global burden of mental health problems among children and adolescents during COVID-19 pandemic: an umbrella review. Psychiatry Res. 2022;317:114814. https://doi.org/10.1016/j.psychres.2022.114814.
Kurdyak P, Patten S. The burden of mental illness and evidence-informed mental health policy development. Can J Psychiatry. 2022;67(2):104–6. https://doi.org/10.1177/07067437211021299.
Stumbrys D, Jasilionis D, Pūras D. The burden of mental health-related mortality in the Baltic States in 2007–2018. BMC Public Health. 2022;22(1):1776. https://doi.org/10.1186/s12889-022-14175-9.
Pompili M, Innamorati M, Gonda X, Serafini G, Sarno S, Erbuto D, et al. Affective temperaments and hopelessness as predictors of health and social functioning in mood disorder patients: a prospective follow-up study. J Affect Disord. 2013;150(2):216–22. https://doi.org/10.1016/j.jad.2013.03.026.
Costanza A, Vasileios C, Ambrosetti J, Shah S, Amerio A, Aguglia A, et al. Demoralization in suicide: a systematic review. J Psychosom Res. 2022;157:110788. https://doi.org/10.1016/j.jpsychores.2022.110788.
Arias F, Szerman N, Vega P, Mesías B, Basurte I, Rentero D. Bipolar disorder and substance use disorders. Madrid study on the prevalence of dual disorders/pathology. Adicciones. 2017;29(3):186–94. https://doi.org/10.2088/adicciones.782.
Brewer S, Godley MD, Hulvershorn LA. Treating mental health and substance use disorders in adolescents: what is on the menu? Curr Psychiatry Rep. 2017;19(1):5. https://doi.org/10.1007/s11920-017-0755-0.
Jones CM, McCance-Katz EF. Co-occurring substance use and mental disorders among adults with opioid use disorder. Drug Alcohol Depend. 2019;197:78–82. https://doi.org/10.1016/j.drugalcdep.2018.12.030.
Murthy P, Mahadevan J, Chand PK. Treatment of substance use disorders with co-occurring severe mental health disorders. Curr Opin Psychiatry. 2019;32(4):293–9. https://doi.org/10.1097/yco.0000000000000510.
Saddichha S, Schütz CG, Sinha BN, Manjunatha N. Substance use and dual diagnosis disorders: future epidemiology, determinants, and policies. Biomed Res Int. 2015;2015:145905. https://doi.org/10.1155/2015/145905.
Hammen C. Adolescent depression: stressful interpersonal contexts and risk for recurrence. Curr Dir Psychol Sci. 2009;18(4):200–4. https://doi.org/10.1111/j.1467-8721.2009.01636.x.
Wolitzky-Taylor K, Bobova L, Zinbarg RE, Mineka S, Craske MG. Longitudinal investigation of the impact of anxiety and mood disorders in adolescence on subsequent substance use disorder onset and vice versa. Addict Behav. 2012;37(8):982–5. https://doi.org/10.1016/j.addbeh.2012.03.026.
Mueser KT, Drake RE, Wallach MA. Dual diagnosis: a review of etiological theories. Addict Behav. 1998;23(6):717–34.
Hartz SM, Pato CN, Medeiros H, Cavazos-Rehg P, Sobell JL, Knowles JA, et al. Comorbidity of severe psychotic disorders with measures of substance use. JAMA Psychiat. 2014;71(3):248–54. https://doi.org/10.1001/jamapsychiatry.2013.3726.
Carroll KM, Kiluk BD, Nich C, Babuscio TA, Brewer JA, Potenza MN, et al. Cognitive function and treatment response in a randomized clinical trial of computer-based training in cognitive-behavioral therapy. Subst Use Misuse. 2011;46(1):23–34. https://doi.org/10.3109/10826084.2011.521069.
Drake RE, Mueser KT. Psychosocial approaches to dual diagnosis. Schizophr Bull. 2000;26(1):105–18. https://doi.org/10.1093/oxfordjournals.schbul.a033429.
Ruggeri M, Leese M, Thornicroft G, Bisoffi G, Tansella M. Definition and prevalence of severe and persistent mental illness. Br J Psychiatry. 2000;177:149–55. https://doi.org/10.1192/bjp.177.2.149.
Reavley NJ, Jorm AF. Stigmatizing attitudes towards people with mental disorders: findings from an Australian national survey of mental health literacy and stigma. Aust N Z J Psychiatry. 2011;45(12):1086–93. https://doi.org/10.3109/00048674.2011.621061.
Torrey WC, Tepper M, Greenwold J. Implementing integrated services for adults with co-occurring substance use disorders and psychiatric illnesses: a research review. J Dual Diagn. 2011;7(3):150–61. https://doi.org/10.1080/15504263.2011.592769.
Bouchery EE, Harwood HJ, Dilonardo J, Vandivort-Warren R. Type of health insurance and the substance abuse treatment gap. J Subst Abuse Treat. 2012;42(3):289–300. https://doi.org/10.1016/j.jsat.2011.09.002.
Abuse S, Administration MHS. National Mental Health Services Survey (N-MHSS): 2014. Data on mental health treatment facilities. Department of Health and Human Services, Substance Abuse and Mental Health …; 2014.
Shiner B, Gottlieb D, Rice K, Forehand JA, Snitkin M, Watts BV. Evaluating policies to improve access to mental health services in rural areas. J Rural Health. 2022;38(4):805–16. https://doi.org/10.1111/jrh.12674.
Ioannidis JP, Greenland S, Hlatky MA, Khoury MJ, Macleod MR, Moher D, et al. Increasing value and reducing waste in research design, conduct, and analysis. Lancet. 2014;383(9912):166–75. https://doi.org/10.1016/s0140-6736(13)62227-8.
Bornmann L, Bowman BF, Bauer J, Marx W, Schier H, Palzenberger MJBbHmiosi. (2014): 11 Bibliometric standards for evaluating research institutes in the natural sciences.201.
Hicks D, Wouters P, Waltman L, de Rijcke S, Rafols I. Bibliometrics: the Leiden manifesto for research metrics. Nature. 2015;520(7548):429–31. https://doi.org/10.1038/520429a.
Ziedonis D, Brady K. Dual diagnosis in primary care. Detecting and treating both the addiction and mental illness. Med Clin North Am. 1997;81(4):1017–36. https://doi.org/10.1016/s0025-7125(05)70561-7.
Kim JI, Kim B, Kim BN, Hong SB, Lee DW, Chung JY, et al. Prevalence of psychiatric disorders, comorbidity patterns, and repeat offending among male juvenile detainees in South Korea: a cross-sectional study. Child Adolesc Psychiatry Ment Health. 2017;11:6. https://doi.org/10.1186/s13034-017-0143-x.
Astals M, Domingo-Salvany A, Buenaventura CC, Tato J, Vazquez JM, Martín-Santos R, et al. Impact of substance dependence and dual diagnosis on the quality of life of heroin users seeking treatment. Subst Use Misuse. 2008;43(5):612–32. https://doi.org/10.1080/10826080701204813.
Buckley PF. Prevalence and consequences of the dual diagnosis of substance abuse and severe mental illness. J Clin Psychiatry. 2006;67(Suppl 7):5–9.
Buckley PF, Brown ES. Prevalence and consequences of dual diagnosis. J Clin Psychiatry. 2006;67(7):e01. https://doi.org/10.4088/jcp.0706e01.
Canaway R, Merkes M. Barriers to comorbidity service delivery: the complexities of dual diagnosis and the need to agree on terminology and conceptual frameworks. Aust Health Rev. 2010;34(3):262–8. https://doi.org/10.1071/ah08723.
Edward KL, Munro I. Nursing considerations for dual diagnosis in mental health. Int J Nurs Pract. 2009;15(2):74–9. https://doi.org/10.1111/j.1440-172X.2009.01731.x.
Healey C, Peters S, Kinderman P, McCracken C, Morriss R. Reasons for substance use in dual diagnosis bipolar disorder and substance use disorders: a qualitative study. J Affect Disord. 2009;113(1–2):118–26. https://doi.org/10.1016/j.jad.2008.05.010.
Horsfall J, Cleary M, Hunt GE, Walter G. Psychosocial treatments for people with co-occurring severe mental illnesses and substance use disorders (dual diagnosis): a review of empirical evidence. Harv Rev Psychiatry. 2009;17(1):24–34. https://doi.org/10.1080/10673220902724599.
Kerfoot KE, Petrakis IL, Rosenheck RA. Dual diagnosis in an aging population: prevalence of psychiatric disorders, comorbid substance abuse, and mental health service utilization in the department of veterans affairs. J Dual Diagn. 2011;7(1–2):4–13. https://doi.org/10.1080/15504263.2011.568306.
Morojele NK, Saban A, Seedat S. Clinical presentations and diagnostic issues in dual diagnosis disorders. Curr Opin Psychiatry. 2012;25(3):181–6. https://doi.org/10.1097/YCO.0b013e328351a429.
Thylstrup B, Johansen KS. Dual diagnosis and psychosocial interventions–introduction and commentary. Nord J Psychiatry. 2009;63(3):202–8. https://doi.org/10.1080/08039480802571069.
van Eck NJ, Waltman L. Software survey: VOSviewer, a computer program for bibliometric mapping. Scientometrics. 2010;84(2):523–38. https://doi.org/10.1007/s11192-009-0146-3.
Arndt S, Tyrrell G, Flaum M, Andreasen NC. Comorbidity of substance abuse and schizophrenia: the role of pre-morbid adjustment. Psychol Med. 1992;22(2):379–88. https://doi.org/10.1017/S0033291700030324.
Barnes TRE, Mutsatsa SH, Hutton SB, Watt HC, Joyce EM. Comorbid substance use and age at onset of schizophrenia. Br J Psychiatry. 2006;188:237–42. https://doi.org/10.1192/bjp.bp.104.007237.
Brady KT, Killeen T, Saladin ME, Dansky B, Becker S. Comorbid substance abuse and posttraumatic stress disorder: characteristics of women in treatment. Am J Addict. 1994;3(2):160–4. https://doi.org/10.1111/j.1521-0391.1994.tb00383.x.
Brière FN, Rohde P, Seeley JR, Klein D, Lewinsohn PM. Comorbidity between major depression and alcohol use disorder from adolescence to adulthood. Compr Psychiatry. 2014;55(3):526–33. https://doi.org/10.1016/j.comppsych.2013.10.007.
Brown PJ, Stout RL, Mueller T. Substance use disorder and posttraumatic stress disorder comorbidity: addiction and psychiatric treatment rates. Psychol Addict Behav. 1999;13(2):115–22. https://doi.org/10.1037/0893-164X.13.2.115.
Bulik CM, Klump KL, Thornton L, Kaplan AS, Devlin B, Fichter MM, et al. Alcohol use disorder comorbidity in eating disorders: a multicenter study. J Clin Psychiatry. 2004;65(7):1000–6. https://doi.org/10.4088/JCP.v65n0718.
Compton WM, Conway KP, Stinson FS, Grant BF. Changes in the prevalence of major depression and comorbid substance use disorders in the United States between 1991–1992 and 2001–2002. Am J Psychiatry. 2006;163(12):2141–7. https://doi.org/10.1176/ajp.2006.163.12.2141.
Green AI, Drake RE, Brunette MF, Noordsy DL. Schizophrenia and co-occurring substance use disorder. Am J Psychiatry. 2007;164(3):402–8. https://doi.org/10.1176/ajp.2007.164.3.402.
Morgenstern J, Langenbucher J, Labouvie E, Miller KJ. The comorbidity of alcoholism and personality disorders in a clinical population: prevalence rates and relation to alcohol typology variables. J Abnorm Psychol. 1997;106(1):74–84. https://doi.org/10.1037/0021-843X.106.1.74.
Back SE, Waldrop AE, Brady KT. Treatment challenges associated with comorbid substance use and posttraumatic stress disorder: clinicians’ perspectives. Am J Addict. 2009;18(1):15–20. https://doi.org/10.1080/10550490802545141.
Brown PJ, Recupero PR, Stout R. PTSD substance abuse comorbidity and treatment utilization. Addict Behav. 1995;20(2):251–4. https://doi.org/10.1016/0306-4603(94)00060-3.
Harris KM, Edlund MJ. Use of mental health care and substance abuse treatment among adults with co-occurring disorders. Psychiatr Serv. 2005;56(8):954–9. https://doi.org/10.1176/appi.ps.56.8.954.
Hien DA, Cohen LR, Miele GM, Litt LC, Capstick C. Promising treatments for women with comorbid PTSD and substance use disorders. Am J Psychiatry. 2004;161(8):1426–32. https://doi.org/10.1176/appi.ajp.161.8.1426.
Manwani SG, Szilagyi KA, Zablotsky B, Hennen J, Griffin ML, Weiss RD. Adherence to pharmacotherapy in bipolar disorder patients with and without co-occurring substance use disorders. J Clin Psychiatry. 2007;68(8):1172–6. https://doi.org/10.4088/JCP.v68n0802.
Minkoff K. An integrated treatment model for dual diagnosis of psychosis and addiction. Hosp Community Psychiatry. 1989;40(10):1031–6. https://doi.org/10.1176/ps.40.10.1031.
Smith JP, Book SW. Comorbidity of generalized anxiety disorder and alcohol use disorders among individuals seeking outpatient substance abuse treatment. Addict Behav. 2010;35(1):42–5. https://doi.org/10.1016/j.addbeh.2009.07.002.
Kamali M, Kelly L, Gervin M, Browne S, Larkin C, O’Callaghan E. The prevalence of comorbid substance misuse and its influence on suicidal ideation among in-patients with schizophrenia. Acta Psychiatr Scand. 2000;101(6):452–6. https://doi.org/10.1034/j.1600-0447.2000.101006452.x.
Padgett DK, Gulcur L, Tsemberis S. Housing first services for people who are homeless with co-occurring serious mental illness and substance abuse. Res Soc Work Pract. 2006;16(1):74–83. https://doi.org/10.1177/1049731505282593.
Schmidt LM, Hesse M, Lykke J. The impact of substance use disorders on the course of schizophrenia-A 15-year follow-up study. Dual diagnosis over 15 years. Schizophr Res. 2011;130(1–3):228–33. https://doi.org/10.1016/j.schres.2011.04.011.
Singh J, Mattoo SK, Sharan P, Basu D. Quality of life and its correlates in patients with dual diagnosis of bipolar affective disorder and substance dependence. Bipolar Disord. 2005;7(2):187–91. https://doi.org/10.1111/j.1399-5618.2004.00173.x.
Urboanoski KA, Cairney J, Bassani DG, Rush BR. Perceived unmet need for mental health care for Canadians with co-occurring mental and substance use disorders. Psychiatr Serv. 2008;59(3):283–9. https://doi.org/10.1176/appi.ps.59.3.283.
Kingston REF, Marel C, Mills KL. A systematic review of the prevalence of comorbid mental health disorders in people presenting for substance use treatment in Australia. Drug Alcohol Rev. 2017;36(4):527–39. https://doi.org/10.1111/dar.12448.
Klinkenberg WD, Caslyn RJ, Morse GA, Yonker RD, McCudden S, Ketema F, et al. Prevalence of human immunodeficiency virus, hepatitis B, and hepatitis C among homeless persons with co-occurring severe mental illness and substance use disorders. Compr Psychiatry. 2003;44(4):293–302. https://doi.org/10.1016/S0010-440X(03)00094-4.
Wallace C, Mullen PE, Burgess P. Criminal offending in schizophrenia over a 25-year period marked by deinstitutionalization and increasing prevalence of comorbid substance use disorders. Am J Psychiatry. 2004;161(4):716–27. https://doi.org/10.1176/appi.ajp.161.4.716.
Bronisch T, Wittchen HU. Suicidal ideation and suicide attempts: comorbidity with depression, anxiety disorders, and substance abuse disorder. Eur Arch Psychiatry Clin Neurosci. 1994;244(2):93–8. https://doi.org/10.1007/BF02193525.
Hatzenbuehler ML, Keyes KM, Narrow WE, Grant BF, Hasin DS. Racial/ethnic disparities in service utilization for individuals with co-occurring mental health and substance use disorders in the general population: Results from the national epidemiologic survey on alcohol and related conditions. J Clin Psychiatry. 2008;69(7):1112–21. https://doi.org/10.4088/JCP.v69n0711.
Hodgins S, Tiihonen J, Ross D. The consequences of conduct disorder for males who develop schizophrenia: associations with criminality, aggressive behavior, substance use, and psychiatric services. Schizophr Res. 2005;78(2–3):323–35. https://doi.org/10.1016/j.schres.2005.05.021.
Hunt GE, Bergen J, Bashir M. Medication compliance and comorbid substance abuse in schizophrenia: impact on community survival 4 years after a relapse. Schizophr Res. 2002;54(3):253–64. https://doi.org/10.1016/S0920-9964(01)00261-4.
Link BG, Struening EL, Rahav M, Phelan JC, Nuttbrock L. On stigma and its consequences: evidence from a longitudinal study of men with dual diagnoses of mental illness and substance abuse. J Health Soc Behav. 1997;38(2):177–90. https://doi.org/10.2307/2955424.
Priester MA, Browne T, Iachini A, Clone S, DeHart D, Seay KD. Treatment access barriers and disparities among individuals with co-occurring mental health and substance use disorders: an integrative literature review. J Subst Abuse Treat. 2016;61:47–59. https://doi.org/10.1016/j.jsat.2015.09.006.
Talamo A, Centorrino F, Tondo L, Dimitri A, Hennen J, Baldessarini RJ. Comorbid substance-use in schizophrenia: relation to positive and negative symptoms. Schizophr Res. 2006;86(1–3):251–5. https://doi.org/10.1016/j.schres.2006.04.004.
Teplin LA, Elkington KS, McClelland GM, Abram KM, Mericle AA, Washburn JJ. Major mental disorders, substance use disorders, comorbidity, and HIV-AIDS risk behaviors in juvenile detainees. Psychiatr Serv. 2005;56(7):823–8. https://doi.org/10.1176/appi.ps.56.7.823.
Hinckley JD, Danielson CK. Elucidating the neurobiologic etiology of comorbid PTSD and substance use disorders. Brain Sci. 2022. https://doi.org/10.3390/brainsci12091166.
Jarnecke AM, Saraiya TC, Brown DG, Richardson J, Killeen T, Back SE. Examining the role of social support in treatment for co-occurring substance use disorder and posttraumatic stress disorder. Addict Behav Rep. 2022. https://doi.org/10.1016/j.abrep.2022.100427.
Kyster NB, Tranberg K, Osler M, Hjorthøj C, Mårtensson S. The influence of childhood aspirations on the risk of developing psychotic disorders, substance use disorders, and dual diagnosis in adulthood based on the Metropolit 1953 Danish male birth cohort. Eur Child Adolesc Psychiatry. 2022. https://doi.org/10.1007/s00787-022-02091-7.
Cunill R, Castells X, González-Pinto A, Arrojo M, Bernardo M, Sáiz PA, et al. Clinical practice guideline on pharmacological and psychological management of adult patients with attention deficit and hyperactivity disorder and comorbid substance use. Adicciones. 2022;34(2):168–78. https://doi.org/10.2088/adicciones.1569.
Margolese HC, Boucher M, Therrien F, Clerzius G. Treatment with aripiprazole once-monthly injectable formulation is effective in improving symptoms and global functioning in schizophrenia with and without comorbid substance use—a post hoc analysis of the ReLiAM study. BMC Psychiatry. 2022. https://doi.org/10.1186/s12888-022-04397-x.
Minkoff K, Covell NH. Recommendations for integrated systems and services for people with co-occurring mental health and substance use conditions. Psychiatric Serv. 2022;73(6):686–9. https://doi.org/10.1176/appi.ps.202000839.
Oliva V, De Prisco M, Pons-Cabrera MT, Guzmán P, Anmella G, Hidalgo-Mazzei D, et al. Machine learning prediction of comorbid substance use disorders among people with bipolar disorder. J Clin Med. 2022. https://doi.org/10.3390/jcm11143935.
Somohano VC, Kaplan J, Newman AG, O’Neil M, Lovejoy T. Formal mindfulness practice predicts reductions in PTSD symptom severity following a mindfulness-based intervention for women with co-occurring PTSD and substance use disorder. Addict Sci Clin Pract. 2022. https://doi.org/10.1186/s13722-022-00333-2.
Watkins LE, Patton SC, Drexler K, Rauch SAM, Rothbaum BO. Clinical effectiveness of an intensive outpatient program for integrated treatment of comorbid substance abuse and mental health disorders. Cogn Behav Pract. 2022. https://doi.org/10.1016/j.cbpra.2022.05.005.
Bertulies-Esposito B, Ouellet-Plamondon C, Jutras-Aswad D, Gagnon J, Abdel-Baki A. The impact of treatment orders for residential treatment of comorbid severe substance use disorders for youth suffering from early psychosis: a case series. Int J Ment Heal Addict. 2021;19(6):2233–44. https://doi.org/10.1007/s11469-020-00317-w.
Butler A, Nicholls T, Samji H, Fabian S, Lavergne MR. Prevalence of mental health needs, substance use, and co-occurring disorders among people admitted to prison. Psychiatric Serv. 2022;73(7):737–44. https://doi.org/10.1176/appi.ps.202000927.
Henderson JL, Wilkins LK, Hawke LD, Wang W, Sanches M, Brownlie EB, et al. Longitudinal emergence of concurrent mental health and substance use concerns in an ontario school-based sample: the research and action for teens study. J Can Acad Child Adolesc Psychiatry. 2021;30(4):249–63.
Huang JS, Yang FC, Chien WC, Yeh TC, Chung CH, Tsai CK, et al. Risk of substance use disorder and its associations with comorbidities and psychotropic agents in patients with autism. JAMA Pediatr. 2021. https://doi.org/10.1001/jamapediatrics.2020.5371.
Lu W, Muñoz-Laboy M, Sohler N, Goodwin RD. Trends and disparities in treatment for co-occurring major depression and substance use disorders among US adolescents from 2011 to 2019. JAMA Netw Open. 2021. https://doi.org/10.1001/jamanetworkopen.2021.30280.
Melkonian AJ, Flanagan JC, Calhoun CD, Hogan JN, Back SE. Craving moderates the effects of intranasal oxytocin on anger in response to social stress among veterans with co-occurring posttraumatic stress disorder and alcohol use disorder. J Clin Psychopharmacol. 2021;41(4):465–9. https://doi.org/10.1097/JCP.0000000000001434.
Otasowie J. Co-occurring mental disorder and substance use disorder in young people: aetiology, assessment and treatment. BJPsych Adv. 2021;27(4):272–81. https://doi.org/10.1192/bja.2020.64.
Saraiya TC, Badour CL, Jones AC, Jarnecke AM, Brown DG, Flanagan JC, et al. The role of posttraumatic guilt and anger in integrated treatment for PTSD and co-occurring substance use disorders among primarily male veterans. Psychol Trauma: Theory Res Pract Policy. 2022. https://doi.org/10.1037/tra0001204.
Walhout SJN, Zanten JV, DeFuentes-Merillas L, Sonneborn CKME, Bosma M. Patients with autism spectrum disorder and co-occurring substance use disorder: a clinical intervention study. Subst Abuse: Res Treat. 2022. https://doi.org/10.1177/11782218221085599.
Walker D, Infante AA, Knight D. Examining the impact of mental health, substance use, and co-occurring disorders on juvenile court outcomes. J Res Crime Delinq. 2022;59(6):820–53. https://doi.org/10.1177/00224278221084981.
Warfield SC, Pack RP, Degenhardt L, Larney S, Bharat C, Ashrafioun L, et al. The next wave? Mental health comorbidities and patients with substance use disorders in under-resourced and rural areas. J Subst Abuse Treat. 2021. https://doi.org/10.1016/j.jsat.2020.108189.
Hien DA, Fitzpatrick S, Saavedra LM, Ebrahimi CT, Norman SB, Tripp J, et al. What’s in a name? A data-driven method to identify optimal psychotherapy classifications to advance treatment research on co-occurring PTSD and substance use disorders. Eur J Psychotraumatol. 2022. https://doi.org/10.1080/20008198.2021.2001191.
Leonhardt M, Brodahl M, Cogan N, Lien L. How did the first COVID-19 lockdown affect persons with concurrent mental health and substance use disorders in Norway? A qualitative study. BMC Psychiatry. 2022. https://doi.org/10.1186/s12888-022-03812-7.
Leonhardt M, Kyrdalen E, Holstad A, Hurlen-Solbakken H, Chiu MYL, Lien L. Norwegian cross-cultural adaptation of the social and communities opportunities profile-mini for persons with concurrent mental health and substance use disorders. J Psychosoc Rehabil Mental Health. 2022. https://doi.org/10.1007/s40737-022-00309-0.
Sell L, Lund HL, Johansen KS. Past, present, and future labor market participation among patients admitted to hospital with concurrent substance use and mental health disorder, and what we can learn from it. J Occup Environ Med. 2022;64(12):1041–5. https://doi.org/10.1097/JOM.0000000000002633.
Sverdlichenko I, Hawke LD, Henderson J. Understanding the service needs of youth with opioid use: a descriptive study of demographics and co-occurring substance use and mental health concerns. J Subst Abuse Treat. 2022. https://doi.org/10.1016/j.jsat.2021.108592.
Yerriah J, Tomita A, Paruk S. Surviving but not thriving: Burden of care and quality of life for caregivers of patients with schizophrenia spectrum disorders and comorbid substance use in South Africa. Early Interv Psychiatry. 2022;16(2):153–61. https://doi.org/10.1111/eip.13141.
Murthy P, Chand P. Treatment of dual diagnosis disorders. Curr Opin Psychiatry. 2012;25(3):194–200. https://doi.org/10.1097/YCO.0b013e328351a3e0.
Schneier M. Better treatment for dual diagnosis patients. Psychiatr Serv. 2000;51(9):1079. https://doi.org/10.1176/appi.ps.51.9.1079.
Tirado Muñoz J, Farré A, Mestre-Pintó J, Szerman N, Torrens M. Dual diagnosis in depression: treatment recommendations. Adicciones. 2018;30(1):66–76. https://doi.org/10.2088/adicciones.868.
Carrà G, Clerici M. Dual diagnosis–policy and practice in Italy. Am J Addict. 2006;15(2):125–30. https://doi.org/10.1080/10550490500528340.
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
W.S started the idea, designed the methodology; did the data analysis, graphics, and data interpretation; wrote and submitted the manuscript. This was a single-authored manuscript. W.S wrote and submitted the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
IRB at An-Najah National University (Palestine) requires no approval for bibliometric studies.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Sweileh, W.M. Research landscape analysis on dual diagnosis of substance use and mental health disorders: key contributors, research hotspots, and emerging research topics. Ann Gen Psychiatry 23, 32 (2024). https://doi.org/10.1186/s12991-024-00517-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12991-024-00517-x